Prioritize access, convenience & efficiency
Work smarter with Fabric’s clinical intelligence engine and adaptive interviews that automate symptom gathering and accelerate diagnosis while triaging and routing patients to in-person care options when appropriate.
Streamline treatment
Save provider time by automating clinical symptom gathering, SOAP notes, and care plans. Fabric’s clinical decision support standardizes processes to ensure quality and antibiotic stewardship.
Prioritize patient & provider time
Enable providers to spend more time with patients who need in-person attention by offloading low-acuity visits to asynchronous telehealth that is 10x faster than video or in-person care.
Increase access
Extend geographic reach and serve patients in rural and disadvantaged populations with an easily accessible solution that doesn’t require high-speed internet access and excels at bit rates that are 86% lower than video.
How it works
So much more than video, Fabric’s async telemedicine platform is smart, adaptive, and efficient.
.png)
24/7 patient access
Patients initiate their care in minutes with a consumer-grade experience that’s available 24/7—365 days a year.
%201%20(1).png)
Clinical symptom gathering
Patients are guided through symptom-specific protocols built by physicians and informaticists and validated by the nearly 20 Chief Medical Officers and MDs that serve on Fabric’s Clinical Quality Advisory Council.
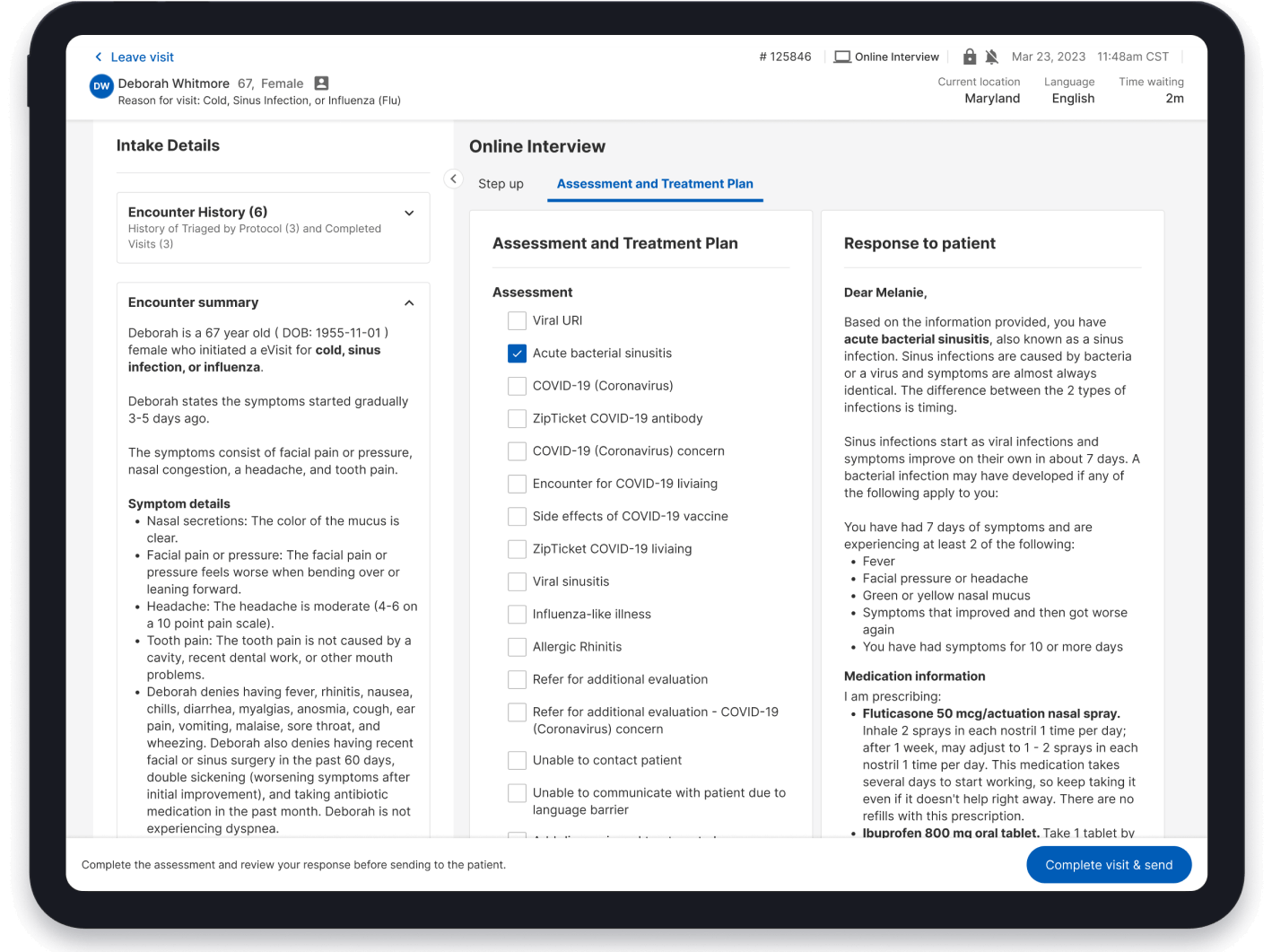
Efficient provider workflows
Physicians receive a pre-populated SOAP note, and clinical decision support enables diagnosis, treatment, and care plans in just two clicks. This process takes 89 seconds of provider time and reduces patient wait time to under 9 minutes.
Proven results
89
seconds of average clinical work time per visit
90%
adherence to clinical guidelines
9
minute average patient wait time
64
patient net promoter score

“I was having major mom guilt. [Fabric] definitely increased time with family. I don’t feel that I have to be behind a computer 24/7. I can put it down. I can go spend time and I know that I’m not going to get so backed up that I feel like I’m drowning.”
Blair Lober, CRNP, Owner
OMNIA TeleHEALTH
Dive deeper
Read through case studies that reinforce our track record, blogs that reflect our expertise, and guides that inform and complement your experience with Fabric.
Part of Fabric’s Hybrid Care solution
Seamlessly guide patients through the entire continuum of care while cutting back on admin tasks, improving the patient experience, and driving revenue.
Virtual Care
Enhance workflows around patient intake, documentation, and symptom collection through powerful automation tools.
Our solution
Synchronous Care
Optimize patient data collection and reduce clinical burden with adaptive interviews, remote patient monitoring, and more.
Our solution
In-Person Care
Automate intake, registration, discharge, and more with advanced routing and scheduling tools.
Our solution
In-Person Care Guides
Streamline the patient, nurse, and provider experiences with real-time updates, attachment to PCPs, and automated patient data collection.
Our solution

Backed by Clinical Content & Automation
Customize clinical protocols to suit your needs to free up clinical staff and guide patients through their care journey.
Loom
Powered by clinical intelligence
Meet Loom, Fabric’s clinical intelligence engine – the expert system, content engine, and conversational AI solution that drives our care enablement platform. Built by clinicians, for clinicians, Loom intelligently captures patient data to identify disposition, triages and routes patients to the right point of care, offers clinical decision support and automates SOAP notes, care plans, and visit summaries.
.png)
An end-to-end solution
Allow clinicians and practitioners to effortlessly see patients through the entirety of their healthcare journey. From intake to treatment all the way to follow-up care.
.jpg)




.svg)
.svg)